Bipolar Affective Disorder 2 and Me
I’ve been feeling a bit lost in the definition of my mental illness recently. It’s fine for other people to say ‘you’re not your diagnosis’ and ‘your diagnosis doesn’t define you’ and I know what they mean, but, when you’ve waited so long to find out what it is that is causing you to feel ‘broken’ it is useful to know how you fit. Think of yourself as a jigsaw, like a floor puzzle and there are only a dozen pieces. One piece has been missing for your whole life and then some one comes along and finds it for you and puts the last piece in and suddenly the picture is complete. What is on that piece is probably important to you, it’s got to match up. Seeing what that piece looks like helps you to complete the picture.
I’ve been getting involved in various support groups nationally and on a local level and joined a Bipolar UK conference this week with over 3000 other people. The more I learn about this condition, the more I feel reassured that I’m not the only one but also I feel more out of touch with my regular life. I decided therefore to write about what I’d like my family and my friends to know about Bipolar. Face to face with people I’m a bit of a blabber mouth and I’ll happily talk about myself but we don’t always have that chance so here we go…….
Bipolar – the facts and stats
- As many as 5% of the UK population may be on the bipolar spectrum
- It’s one of the UK’s commonest long term health conditions
- It takes an average of 9 years to get a correct diagnosis of bipolar (for me I think it has taken 17, that is when I was first officially treated for a mental health condition, not how long I’ve had bipolar symptoms)
- Bipolar increases an individuals risk of suicide by up to 20 times, it is estimated that 50% of all suicides are linked to an underlying bipolar condition
- Bipolar is more treatable than many other mental health conditions if diagnosed and managed correctly
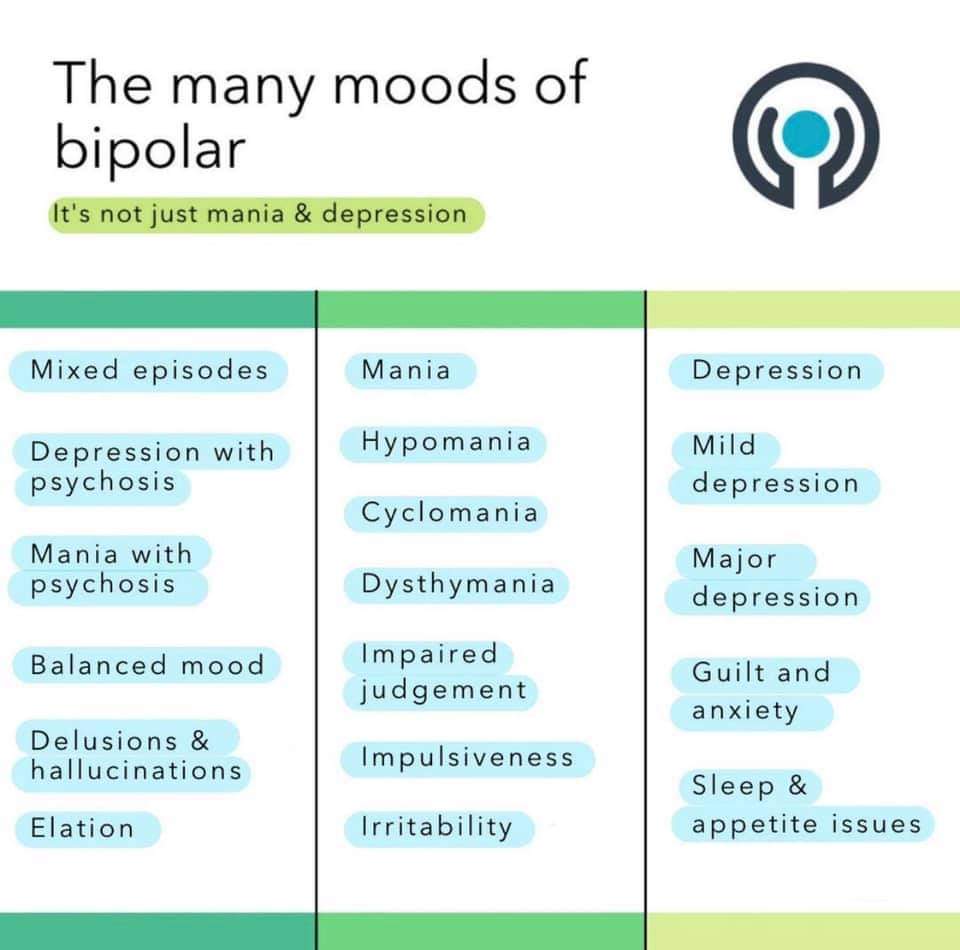
Bipolar is a mental illness characterised by extreme moods. I think the diagram below shows it perfectly.
The average person (in dark red) has mood swings up and down affected by life experiences, hormones etc.
Someone with depression (in yellow) will have normal moods but with some depressive states.
Bipolar 1 (in light blue) has extreme moods.
Bipolar 2 (in light green) has deep lows, actually deeper typically than BP1 and slightly more extreme highs than the average person.
Cyclothymia (dark blue) is similar to BP2 but the cycle varies more rapidly and mood isn’t always as low.
The problem with a mental illness like Bipolar is that often your moods don’t correspond with what is going on in your life. They’re also closely tied with energy. So you can wake up having had a great sleep and no external issues but feel extremely low. These extreme moods don’t follow a pattern although they can be triggered by stress, alcohol or drugs.
I do get some good periods of stability but even then I wait for the next extreme mood. Also, when you’re stable you often feel like an imposter and think your diagnosis is wrong, this is when many people stop taking their medication and then trigger an extreme mood.
I am learning to spot the signs of different extreme moods or episodes. For example:
Depression – I become tearful, need much more sleep, start to struggle with memory and logistics, start to withdraw from social interaction, activity such as running becomes much harder. Drinking alcohol would make me very low at this time.
Hypomania – I sleep a bit less, have lots of ideas for writing, making things and changing the house. I’m very chatty and interact well socially, take on roles and responsibilities. I can run easily and build up my distance. I am impulsive and will spend money or make decisions that I later possibly regret. I might be more argumentative and more present on social media. I also have psychotic episodes in the form of delusions in this state.
The worst times for me are ‘mixed episodes’. These are when my depression is bad but my energy is high. So I will seem like I’m interacting well but I am not well at all. I will sleep as little as 4 hours a night and be okay with that, I will be jittery and talk a lot, my appetite goes completely. I am happy to take things on and do a lot. This is when I was in danger of binge drinking but also had suicidal thoughts and became impulsive. Psychotic thoughts are also present in this state. This is the most frightening episode but thankfully the rarest.
At this point I want to talk about the language we use for describing mental health. We use a lot of the lexicon very flippantly day to day, using words that the psychiatric community have specific meanings for. Many of the words used have very negative connotations.
For example; manic is used to mean ‘busy’ but a BP1 sufferer in a manic state is actually very poorly and often psychotic.
Psychotic we use to mean ‘dangerous’ but actually very, very few people with mental illness with pyschosis are a danger to anyone else.
When someone is suffering psychosis they may have delusions in the form of hallucinations. We often think hallucinations mean ‘visual disturbances’. In fact, an hallucination can affect any of your five senses. You could feel like ants are crawling up your legs, hear someone shouting a warning at you, smell a bad smell and think it is you or something in your house…..any sense can be affected.
Delusions mean you believe something that is not real and not true. A person might believe they are very powerful or being followed. So this is closely linked to paranoia.
Day to day living with Bipolar can be like being a different person depending on where you are in the mood cycle. Everyday you wake up and wonder how you’re going to feel or if you’re moving into a new episode. Some days I wake up and feel ‘normal’, I still take my medication and I still have to try and follow a routine. Routine, especially around sleep is very important. Some days I wake up and my head literally feels ‘broken’. It’s not that I’m depressed, it’s that I can’t process things easily. This is what makes things like paperwork and logistics and holding down a job difficult for bipolar sufferers. I also have a really bad memory when I’m in any state other than stable. I listen and join in conversations but don’t retain the details. This is also my excuse for never being able to follow any crime dramas!
I try to keep a good sleep routine and try to eat a balanced diet and try to exercise however I feel. I’ve also given up alcohol as it doesn’t mix with the medications and made my moods more extreme. But there are still times that an episode creeps in and I can’t stop it. Sleep isn’t only a vital part of routine, it is also a coping mechanism. I will often go off for an afternoon or early evening nap when we are away or with other people because it gives me a break.
Hypomania generally feels really good, I like who I am and I enjoy the interaction and ideas that I get. I am only just learning to manage these periods as well and not let them get out of hand or wear me out because as great as they are they are usually followed by a deep low. It doesn’t feel right to limit my social contact at this time but I need to say ‘no’ more to stop myself from getting poorly.
The deep lows are awful. They make you feel hopeless, worthless, shame, guilt; it’s the devil on your shoulder whispering incessant criticisms. These periods and mixed episodes are also when BP sufferers are most at risk of self harm and suicide. The more experience I get of talking to other BP sufferers, the more I understand that these are part of the illness and it’s okay to talk about them. We think self harm is limited to teenagers cutting but it’s not. There are plenty of adults using self harm as a coping mechanism whether it’s cutting, burning, banging or using substances. It can be frightening if someone talks about this stuff but talking about it makes it less scary for the sufferer as all of a sudden they are not on their own with it.
I’ve talked about some of the holistic ways of managing the illness but there is of course medication as well. Most people with BP1 or BP2 are treated with a combination of drugs and it can take a while to see what they can tolerate and what helps and what timings and quantities are needed. There are antidepressants (SSRIs and Tricyclics), Mood Stabilisers and AntiPsychotics. This is the psychiatrists job to find what works. My experience of the meds hasn’t been good so far so we’re still working on finding the right combination. They have caused hypermania, mixed episodes, weight loss, weight gain, sickness, fainting, insomnia, extreme tiredness and a high level of liver toxicity!

So how do I feel about having Bipolar? I feel relieved to have a diagnosis and extremely grateful to have the experts and support that I do have around me in the form of my counsellor, psychiatrist and GP. I just needed my family and friends to understand a bit more about it as well. I’m taking my medication, trying to manage my transitions into different moods and making efforts to keep myself safe and healthy for my children. I hope that as I get older and we find the right combination of medications that I will start to have longer periods of stability. Every day I am grappling in some way with how I am, even on the ‘good’ days. There is a certain level of ‘acceptance’ that I’ve got to but some days it’s really hard. Ultimately if I didn’t have Bipolar I might not have the extremely creative bouts of productivity that I get and if one day my novel gets published, then bipolar will receive an acknowledgement!
